This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome."
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE PRESENTATION
A 14 year old male patient came hailing from nalgonda came to the OPD reffered from local hospital 3 days back with cheif complains of
Cough since 8days,
Fever since 8 days,
Shortness of breath since 5 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 8 days back.
Because it was summer his mother let him play in water with his friends and the next day he developed fever followed by cough and shortness of breath.
The fever was mild and not associated with chills and rigor but no evening rise of temperature. The fever relieves on medication.
The cough was not associated any expectoration which was insidious in onset amd non progressive. There were no aggravating or relieving factors or no positional variation.
H/O Shortness of breath since 5days which progressed from MMRC grade 1 to 2. Shortness of breath on exertion and cough and relieved in sitting position
H/O loss of appetite
No chest pain
No loss of consciousness.
No H/o cyanosis.
No H/o orthopnea and PND.
No H/o wheezing.
Not associated with chest pain or confusion or loss of consciousness or headache or loss of weight or night sweats or joint pains or burning micturition
PAST HISTORY:
Patient is a known case of asthma since he was 6 years old
TREATMENT HISTORY: On antiasthmatics since he was 6 year old (budecort and asthalin).
As the drugs dint work this time the child was brought to the hospital.
Not a know case of tuberculosis, diabetes, hypertension, epilepsy, cardiovascular anomalies or renal anomalies.
No past surgical history.
PERSONAL HISTORY:
Diet: Mixed
Appetite: Reduced since the fever
Sleep: The symptoms not disturbing sleep(day time symptoms)
Bowel and bladder movements: Regular
Addictions: None
Allergies: None.
BIRTH HISTORY:
Normal vaginal delivery.
Uneventful pregnancy.
FAMILY HISTORY:
No simialr complaints in the family.
GENRAL EXAMINATION:
Patient is consious, coherent, cooperative and moderately built and moderately nourished.
He is comfortably lying on the couch.
There are no signs of pallor, icterus, koilonychia, clubbing, cyanosis, lymphadenopathy, edema.
VITALS:
Temperature: Afebrile
Blood pressure: 110/70 mmHg
Respiratory rate: 17 cpm
Pulse rate: 90 bpm.
SYSTEMIC EXAMINATION:
Cardiovascular system:
S1 and S2 heard
No murmurs
Apex beat heard in the 5th intercoastalspace
Central nervous system:
Higher mental functions-normal.
Cranial nerves- intact.
Sensory system- normal.
Motor system- normal.
Per abdomen:
All quadrants move with respiration.
No presence of any scars or sinuses or engorged veins.
LOCAL EXAMINATION: Respiratory system:
INSPECTION:
• Shape of the chest: elliptical
• Movements: symmetrical bilaterally
• Drooping of shoulders: absent
• Trachea: central
• Apex beat: not seen
• No presence of any scar, sinuses or dilated veins.
• No use of accessory muscles of respiration
• No Supra or infra clavicular hollowness or fullness
• No drooping of shoulder
• No crowding of ribs
• No wasting of muscles
PALPATION:
• No local rise in temperature and no tenderness
• All inspectory findings confirmed by palpation.
• Trachea : central- confirmed by three finger test.
• Chest movements decreased on left side
• Apex beat:left 5th intercoastalspace 1cm to the medial to MCL
• Tactile vocal phremitus -decreased on left infra scapular.
AUSCULTATION:
• Decreased breath sounds on left side in the Infrascapular area
• Normal vescicular breath sounds heard on the right side.
PERCUSSION:
• Stony dull node is heard on the left Infrascapular area.
• Normal resonant node on the right side.
PROVISIONAL DIAGNOSIS:
Mild left sided pleural effusion.
INVESTIGATIONS:
• Haemogram: Slight decrease in haemoglobin
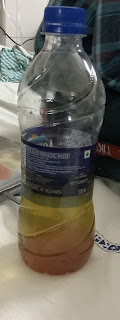
• Thoracocentesis:
Pleural fluid: sugar and protein normal
Serum protein and LDH Levels: Decreased
ACCORDING TO LIGHTS CRITERIA:
Pleural LDH: Serum LDH= 692:196 => 3
Hence the pleural fluid is EXUDATIVE.
ECG:
In case of moderate to severe pleural effusion:
Consider tube thoracostomy and Pleurodesis.